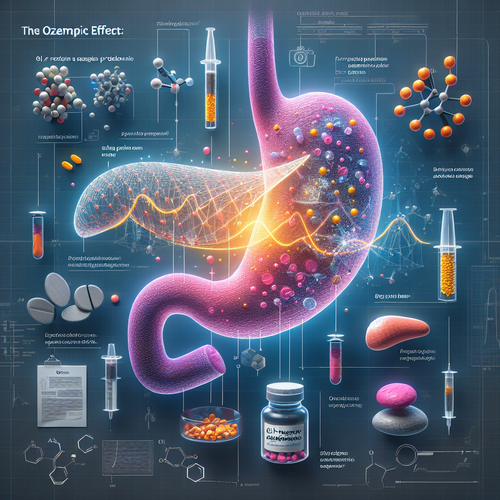
The rapid rise of GLP-1 receptor agonists – drugs like semaglutide, perhaps better known by brand names like Ozempic or Wegovy – has been nothing short of a medical phenomenon. Initially developed for type 2 diabetes management, their remarkable efficacy in promoting significant weight loss quickly propelled them into the mainstream, often hailed as a revolutionary answer to obesity. Social media buzz, celebrity endorsements, and undeniable patient results fueled a global demand, creating a landscape where accessing these medications became a challenge due to sheer popularity. For many struggling with weight-related health issues, these drugs represent a new frontier of hope, offering outcomes previously unimaginable without drastic surgical intervention. However, as with any powerful medical tool adopted on a massive scale, this widespread usage inevitably brings a sharper focus on potential side effects, even rare ones. The honeymoon phase of this medical marvel may now be giving way to a more cautious examination, as regulatory bodies begin to investigate concerning signals emerging from real-world data.
Alarm bells are starting to ring in the United Kingdom, where the Medicines and Healthcare Products Regulatory Agency (MHRA) has launched a significant investigation into reports of acute pancreatitis associated with GLP-1 drug use. This isn’t merely anecdotal chatter; the MHRA’s move is prompted by a noticeable upturn in reported cases, specifically linking these popular weight-loss medications to serious pancreas problems. Hundreds of complaints have reportedly been filed, with a worrying concentration of documented cases emerging in 2025 alone. The UK’s “Yellow Card” system, a crucial mechanism for reporting suspected adverse drug reactions, is reflecting this trend, indicating an increase in reports mentioning GLP-1s and acute pancreatitis. What makes this investigation particularly noteworthy is the collaboration between the MHRA and Genomics England. Their joint effort signals a deeper dive beyond simple correlation, aiming to explore whether an individual’s genetic makeup might predispose them to this specific, severe side effect. This innovative approach hints at a future where understanding our personal genetic code could be key to predicting drug safety.
The reality of pharmacology dictates that every medication, no matter how beneficial, carries potential risks. The sheer scale of GLP-1 adoption means that even side effects occurring in a small percentage of users can translate to a significant number of affected individuals. Pancreatitis, an inflammation of the pancreas, can range from mild discomfort to a life-threatening condition requiring hospitalization. The reported increase, though still being investigated for definitive causality, highlights a critical aspect of post-market drug surveillance. While clinical trials assess safety in controlled populations, widespread use in diverse, real-world patients often reveals rarer or previously undetected adverse events. The MHRA’s investigation, particularly its focus on genetics, represents a proactive step towards understanding *why* some individuals might be vulnerable while others are not. This moves beyond simply listing potential side effects and delves into the biological mechanisms and inherited traits that could influence drug response and safety profiles, potentially paving the way for more personalized prescribing practices.
For the millions currently using or considering GLP-1 drugs for weight management or diabetes, this investigation understandably raises questions. It underscores the vital importance of patient-physician communication and informed consent. Patients should be aware of potential risks, including symptoms like severe abdominal pain that could indicate pancreatitis, and report any concerning issues promptly through systems like the Yellow Card scheme. Regulatory agencies like the MHRA play a critical role in monitoring drug safety *after* they hit the market, acting as vigilant guardians of public health by continuously evaluating real-world data. This ongoing surveillance is a cornerstone of pharmacovigilance, a layer of protection often invisible to the public but essential for ensuring that the benefits of medications continue to outweigh their risks as we learn more about their effects across broader populations and diverse genetic backgrounds. The current investigation is a testament to this continuous learning process.
Looking ahead, the findings of the MHRA and Genomics England investigation could have far-reaching implications. If a genetic link is established, it could fundamentally change how GLP-1 drugs are prescribed, potentially involving genetic screening to identify high-risk individuals. This aligns with the broader trend towards personalized medicine, where treatments are tailored to individual genetic profiles. Regardless of the outcome, this situation serves as a potent reminder that even the most promising medical advancements require ongoing scrutiny and vigilance. The widespread enthusiasm for weight-loss drugs is understandable given the pressing public health challenge of obesity, but it must be tempered with a sober assessment of risks and a commitment to robust safety monitoring. The investigation into GLP-1s and pancreatitis is a crucial step in ensuring that the pursuit of better health outcomes doesn’t inadvertently expose vulnerable individuals to serious harm.
The story of GLP-1 drugs is still unfolding. They have revolutionized weight management for many, but the emerging signals of potential adverse effects like pancreatitis necessitate careful investigation and a balanced perspective. The collaboration between regulatory science and genomics holds the promise of not just identifying risks, but understanding *who* is most at risk, moving us closer to an era of truly personalized and safer medicine. As this investigation progresses, the medical community, regulators, and patients must remain engaged and informed, navigating the complexities of these powerful new tools with caution and a commitment to safety first. The ultimate goal is to harness the benefits of innovation while minimizing unforeseen consequences, ensuring that the promise of these medications is realized responsibly.